TILTed in China
China’s air pollution is so bad that I can imagine doctors’ offices there are filled with sick people. And I suspect many patients have TILT, and they won’t be diagnosed correctly or get well.
 |
|
China unfortunately is a perfect environment for TILT. Years of economic expansion have polluted waterways and loaded the air with contaminants. |
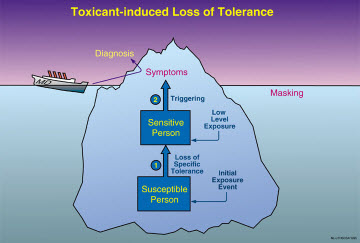
TILT is a disorder caused by exposure to harmful chemicals. The chemical exposures can be at constant low levels, such as in China, or result from an acute event such as exposure to a pesticide.
TILT is short for “Toxicant-induced Loss of Tolerance,” and it indeed represents a breakdown in the body’s natural tolerance. People with TILT can become sick from everyday chemicals in foods, household cleaners and medications.
Sufferers may complain of fatigue, headaches, asthma-like symptoms, and cognitive disorders. But conventional treatments for their symptoms will be ineffective if they have TILT.
For this reason, I worry about the Chinese people because I suspect most health caregivers in China don’t know about TILT, or the widely used clinical screening instrument to identify it. I helped develop the instrument, called the “Quick Environmental Exposure and Sensitivity Inventory,” or QEESI, and it can lead to much better identification and treatment of TILTed patients.
It’s a free download on my website.
QEESI is a clinical assessment tool used in the United States, and it has been translated into French and Korean. Clinicians in South Korea, which also has serious pollution issues, are using the recently-translated version.
China unfortunately is a perfect environment for TILT. Years of economic expansion have polluted waterways and loaded the air with contaminants. Airlines in the past have canceled flights due to poor visibility, pedestrians in cities wear masks, household air purifiers are a status symbol, fishermen report low catches, and civil unrest has forced delay of a coal-fired power plant that residents blame for a rising number of cancer cases.
Soaring levels of pollution are driving Western business executives out of Chinese cities and dissuading others from coming, the Wall Street Journal reported in April.
What is troublesome to medical scientists is the nature of the air pollution. It’s largely unmeasured even though it blots out the sun on some days and residents have been quoted to say they can taste the air. For physicians, it’s difficult to connect an illness to pollution because the measurement of pollution is inadequate.
The Chinese government index of pollution reports only large particulate pollutants, those known as PM 10. They are 10 micrometers in diameter or larger. PM10 particulate is nowhere as dangerous as smaller particulate matter.
China’s government, acting to tighten air pollution standards, began to monitor small particles in January 2012. The state media said the government would begin to measure PM 2.5 and smaller, and publish its measurements.
Despite this, the levels of two major air pollutants rose by almost 30 percent during January-March 2013 over the same period in 2012, a Chinese news organization recently reported. The pollutants were nitrogen dioxide and particulate matter that is between 2.5 and 10 micrometers in diameter, called PM 10.
Small particles can lodge in the alveoli while large particles usually are cleared out in the nasal passages. PM 2.5 is a common byproduct of power plants and motor traffic.
China in the past has been embarrassed by discrepancies between its pollution reports and measurements published by the U.S. Embassy in Beijing. Embassy readings measure PM 2.5, and on some days the measurements have been “beyond index,” or literally off the chart, while the official reading was “light.”
The embassy publishes its measurements, taken on the office rooftop, on Twitter.
In fact, the tweets were cited as a reason the Chinese government in 2012 also recanted an earlier announcement that it would not release the newer, more precise measurements.
Until all the measurements are public, the only generally known element is that the pollution poses immediate danger to the Chinese people, and nearly everyone knows it. The New York Times has quoted a source who said more than 200 high-end air purifiers have been deployed to the office of China’s president, the Zhongnanhai compound for senior government leaders, and the Great Hall of the People.