|
|
Guest blogger Laura MacCleery describes her do-it-yourself room painting project and things you should know before painting a room. Laura is a lawyer, mother and self-described “squeaky wheel in search of a spoke.” She writes commentary at Laura’s Rules. Her post first appeared there on Feb. 1.
|
By Laura MacCleery
What to do with a low-ceilinged, windowless basement room? Give it to the toddler, of course …
But then, it just screams for some cheer. When my friend Lisa showed me the charming mural she had painted on her son’s wall in honor of his adoption, it was inspiring. She told me how she made the cute and life-like clouds using nothing more than a sea sponge and some water-based tempera paint.
I could do that, I thought. So sometime in my feverish, flu-like state, after days of uselessly prowling the house over the holidays, I determined to accomplish some little thing, at least.
The most manageable (and thoughtless) project on my list was introducing a little whimsy to the “playroom.” It mainly functions as a toy storage area these days, given Maya’s inability to be in the basement by her lonesome. But I have hopes, my friends, that someday she will be capable of independent play, and so this is for that day.
First, because it’s me and this blog and all, I must point out what you know already: paint is notoriously toxic. This is a particular concern in a poorly ventilated basement. As the wonderful Diane MacEachern of Big Green Purse (another Takoma Park green blogger!), writes:
Conventional paint contains many volatile organic compounds, or VOCs, that “outgas” and escape into the air after they are applied. Indoors, these VOCs cause headaches, nausea, achy bones, and general discomfort. Outdoors, they contribute to smog and air pollution.
And they smell nasty, which can’t be good. The VOCs include chemicals like terpenes, formaldehyde, acrolein, phthalates, glycol, toluene, methylene chloride, styrene, trichloroethylene, xylenes, and benzene, among others. Any one of these is enough to make me gag, personally. A terrific new guide to building a non-toxic nursery, out just today from our friends at Healthy Child, Healthy World, provides very helpful information about paint types suitable for a nursery or other rooms on p. 16 of their new, interactive ebook and less toxic options. They also have 7 helpful tips for healthier painting. Basically, the best way to go is real zero-VOC paints (i.e., ones that completely and verifiably lack toxics or solvents), or with natural, organic or milk-based paints.
Our local hardware store only stocks the zero-VOC kind, but they at least have a really good brand — Mythic, which I have used on several rooms in our house with excellent results. Mythic is a “real” zero-VOC paint, with no toxics like lead or other known toxins in it, and is also solvent free and it goes on beautifully.
In fact, it’s so clean, it doesn’t need a warning label like most paints. (Lullaby Paints appears to be another great option, but I have not used them myself.) Even using Mythic, I set up a fan to speed the paint drying process, open a window when possible, and do not use the room for at least several days.
Before painting, you should also be aware that many, if not most, paints labeled “zero-VOC” can be problematic, because the colorants still contain VOCs and once they are added, then the paint is “zero-VOC” no longer.
In fact, the Federal Trade Commission just sued Sherwin Williams over false claims on this issue, and won, sort of. The companies now at least have to say, somewhere, that the zero-VOC claim applies only to the base paint and that the VOC levels can be impacted by the dyes. From The Consumerist:
In truth and in fact, in numerous instances, Pure Performance paints do not contain zero VOCs after color is added,” alleged the FTC.
To settle these claims by the agency, both paint companies are prohibited from claiming their paints contain “zero VOCs,” unless, after tinting, they have a VOC level of zero grams per liter.
The companies can continue claiming “zero VOC” if they “clearly and prominently disclose” that the “zero VOC” statement applies only
to the base paint, and that depending on the consumer’s color choice, the VOC level may rise.
At any rate, back to the fun part. For the playroom, I first painted one wall and a strip of a wall in a bright, sunny yellow. One coat was enough to do it. Then, I covered the ceiling in a light blue paint left over from a sample I considered using for Maya’s upstairs room (Ocean Falls was the color). (Yes, her bedroom is blue. And lovely.)
I didn’t bother taping for the ceiling, as the indistinct edges add to the effect. Mythic is also forgiving; a wet sponge used soon after painting will clean up any messes.
Then, using the sea sponge and a pool of paint in the pan, I painted swirls in large circles across the ceiling with a slightly darker blue, called Peace River.
Last, I added white clouds around the lights and all over the ceiling in various sizes using the sponge dipped in Crayola white tempera paint. This can also be easily fixed with a wet sponge while the paint remains wet. I tried to leave a little extra paint in some places for a slight texture.
I was pleased with the result, which adds a dreamy quality to a small, boxy room. And Maya likes it too!
|
|
|
|
Tags:
Big Green purse,
Business,
ceiling,
chemicals,
Child,
children,
clouds,
Consumerist,
Crayola,
decor,
decorations,
DIY,
easy,
eco-,
environmental health,
Family,
Federal Trade Commission,
green,
health,
healthy,
Healthy Child,
Healthy World,
Home,
infancy,
Infant,
infants,
low-VOC,
Lullaby,
mommy blog,
mythic,
Nature,
nursery,
organic,
Paint,
Parent,
parenting,
parents,
playroom,
safety,
sea sponge,
Sherwin Williams,
simple,
sky,
sponge painting,
toddler,
tots,
Toxic,
toxic chemicals,
toxics,
voc,
Volatile organic compound,
wall,
zero-VOC Category:
Health |
Comment
December 19, 2012, 6:09 pm
The Japanese cedar was never known to cause allergic rhinitis in Japan until the 1960s even though the tree had been indigenous to Japan for more than a million years. Recognition of cedar-induced rhinitis and an increase in cases in Japan coincided with lenient regulation of diesel exhaust and increased numbers of diesel vehicles in that country.
What does cedar (really a juniper) allergy have to do with diesel exhaust? Exposure to petrochemicals such diesel exhaust, can lower a person’s tolerance for “natural” substances such as pollen, mold, dust mites and animal dander, leading to allergic reactions. Researchers in Japan have confirmed that exposing mice to diesel exhaust increases their IgE production, the immunoglobulin associated with allergy.
What does this have to do with TILT, or Toxicant-induced Loss of Tolerance? People who become chemically intolerant, or TILTed, frequently report amplified allergic responses. This relationship may help explain the rise in allergic rhinitis in Japan. It explains why the QEESI, or Quick Environmental Exposure and Sensitivity Inventory, asks about a person’s exposures to diesel exhaust and any associated heightened allergic responses.
I know how potent cedar pollen can be. I live in Central Texas, on the edge of the scenic Texas Hill Country. Despite its beauty, the Hill Country has hundreds of thousands of Texas Mountain Cedars that shed notoriously allergenic pollen. From December to February, the pollen causes such severe symptoms that sufferers call it “cedar fever.”
Tags:
allergen,
allergies,
cedar,
cedar fever,
diesel exhaust,
Hill Country,
IgE,
immunoglobulin,
juniper,
pollen,
QEESI,
Quick Environmental Exposure and Sensitivity Inventory,
rhinitis,
Texas,
tilt,
toxicant-induced loss of tolerance Category:
Health |
Comment
December 14, 2012, 7:33 pm
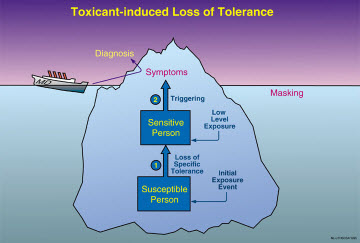
The shooting tragedy at Sandy Hook Elementary School in Newtown, Conn., underscores the urgency for mental health practitioners to understand the TILT iceberg. The iceberg is a graphical depiction of the risks for people with Toxicant-induced Loss of Tolerance.
Practitioners need to take a proper history of their patients and think about the role of petrochemicals/drug exposures in violence. These hair-trigger anger reactions were not uncommon among chemically-exposed Gulf War veterans I saw as a consultant for the Veterans Administration. The veterans had become chemically intolerant and were so afraid they might harm their own families that they gave their guns to friends for safe-keeping.
Dietary intolerances are one of the main consequences of TILT, based upon our extensive studies of people who became ill following exposure to pesticides, solvents, substances used in remodeling, and Gulf War chemicals.
Prisons are controlled environments in which it’s been shown that reducing exposures, even to such benign chemical substances as sugar, can reduce violence.
Read an in-depth exploration in the book I co-authored,
Chemical Exposures: Low Levels and High Stakes.
The Sandy Hook shootings, like those earlier in Oregon, Colorado and elsewhere, appear random but individuals whose limbic systems have been sensitized by exposures and then are triggered by cleaning agents, foods or medications they no longer can tolerate are more likely to pick up a gun and use it.
Using the QEESI, or Quick Environmental Exposure and Sensitivity Inventory, with patients and reducing exposures (pesticides, solvents, etc.) could help. TILT may be responsible for a small subset or a large number of cases, but almost no mental health professionals are aware of this illness dynamic/new paradigm and they must not miss the diagnosis. Too many lives are at stake.
Tags:
cause,
chemical exposure,
Chemical intolerance,
Connecticut,
environmental,
food intolerance,
Gulf War,
guns,
mental health,
mental instability,
Newtown,
psychiatrists,
psychologists,
QEESI,
Sandy Hook,
shootings,
social workers,
tilt,
violence,
weapons Category:
Health |
Comment
December 5, 2012, 6:48 pm
 |
|
Describing preparations for Hurricane Sandy, guest blogger Laura MacCleery gives a humorous example of the old adage about how “no good deed goes unpunished.” Laura is a lawyer, mother and self-described “squeaky wheel in search of a spoke.” She writes commentary at Laura’s Rules.
|
By Laura MacCleery
When I recently filled out a helpful questionnaire on chemical intolerance, the Quick Environmental Exposure and Sensitivity Inventory (QEESI), or “Queasy” as I like to call it among friends, a screw-shaped light bulb went off. (Compact fluorescent, of course.)
According to the results of this scientifically validated tool for measuring sensitivities to toxins in our environment, I am on the “high” end for both exposures and symptoms, meaning that I don’t tolerate smells like gasoline and off-gassing furniture well.
The survey powerfully showed why I obsess about such things, while other people may shrug them off. Seeing how I scored was important to me because it identified some common sources for the headaches and other discomfort I often experience following exposure to an unpleasant chemical-laden odor.
Most of the things on the list on the QEESI, which is a quick inventory, as the name implies, including bleach-based cleaning supplies or a “new car” smell, can make me feel a bit off, even in small doses. I still remember being newly pregnant in a Washington, D.C., wintertime and driving with the windows way down, the cold wind in my face, because freezing was far preferable to the vinyl smell emanating from my brand-new Nissan, especially given my bionic nose from the pregnancy!
But that sensitivity hasn’t gone away since I had my daughter, either. And I’m not the only one who’s bothered by the fragrances crowding our environment. A recent article in a UK newspaper notes that: “One leading expert suggests nearly a third of people suffer adverse health effects from being exposed to scents.”
The article explains:
“Allergies are on the increase, and the amount of perfumed products is also on the rise,” says Dr. Susannah Baron, consultant dermatologist at Kent & Canterbury hospital, and BMI Chaucer Hospital. “Fragrance allergy can show up as contact dermatitis in the site a perfumed product is applied, or as a flare-up of existing eczema. It can be a real problem.” … Often it may not be immediately obvious that you’ve developed a fragrance allergy, says Dr. Baron. “You don’t react immediately; the body notes that it does not like the chemical and develops ‘memory cells,’ which cause inflammation when the body is next exposed to this chemical. Gradually, as you are exposed more and more, the body ramps up its reaction, until it becomes more noticeable to you.”
As the designer of the QEESI tool, Dr. Claudia Miller, an immunologist/allergist, explains based on her many years of research, that biological response is to the chemicals being used to produce the fragrances. Her pioneering work shows that exposures to chemicals of all kinds – not just the smelly ones – can and do trigger a loss of tolerance in some people, causing ill health.
And the simplest things can lead to new exposures, such as our recent utterly ridiculous adventures with installing a generator for our home. We often lose power, and so the prospect of Hurricane Sandy barreling down on us caused a run to the store and triggered a panicky purchase of a generator to help see us through.
Turned out we didn’t need to use it, and instead bought ourselves a world of trouble. In fact, what I didn’t know about it can be counted on all my fingers and toes in the dark, including the substantial extra costs of having an electrician hook it up properly, and the excruciating task of filling tanks up with gasoline, poised over the wafting fumes to ensure that I didn’t overfill the tanks and spill it all on my shoes.
To complete the misadventure, a small amount of gasoline did spill inside my car, rendering it nastily smelly once more. To get the odor out, I tried everything – wiping it down with baby oil, auto cleaners, and baking soda. Repeatedly.
Then I finally took it to a detail shop, and paid them a small fortune to use completely toxic cleaning supplies on the floor and seats. The smell has diminished, but it’s not gone, and it’s mingling with all the cleaners for a soupier feel. I still drive with the windows open and leave them all cracked while parked, at least when there’s no rain coming.
Contrary to what most folks think when they imagine what we are doing to “the environment,” indoor air is far more polluted than that outdoors. Given the number of people whose symptoms have been identified by the QEESI, I don’t think I’m alone in thinking that something is very wrong when the places we build – to live in, no less – are not particularly safe or comfortable for at least some living things.
So if you are like me, and these kinds of odors bother you as you go about your day-to-day, you may want to take the QEESI and see how and why they may be impacting you. And to learn what may be “masking” their effects, so that you don’t know where the headaches are coming from.
Even more pointedly, suppose you go on vacation and get a break from these exposures and feel suddenly better, which happened to a friend of mine, then you may want to start clearing your house of odoriferous chemicals and plastics to see if it makes a difference. It certainly did for her.
On the other hand, if you’re one of the lucky ones who feels just fine in this man-made world of olfactory offenders, well, then, you can snicker at us anti-chemical folk if you’d like to. But you may also want to think about whether those of us with the higher QEESI scores – and the concomitant fascination with “greening” our homes – are actually canaries in a mineshaft.
Tweet, tweet, I say, a bit sadly.
And because I’m a modern bird: Retweet? Are you a canary too?
October 29, 2012, 9:56 am
Dr. Nicholas Ashford, my co-author of the book Chemical Exposures: Low Levels and High Stakes, presented a thought-provoking analogy about how the same chemical exposure can affect people differently. His comments came at a National Academy of Sciences workshop in April 2012. I presented at the same workshop on TILT, or Toxicant-induced Loss of Tolerance; the QEESI, or Quick Environmental Exposure and Sensitivity Inventory; and the need for EMUs, or environmental medical units.
Here are Dr. Ashford’s remarks:
“Let me ask you to do a thought experiment. Suppose there were 10 Apple computers lined up along that front table and I were to open the motherboards of all those computers. Now suppose I were to take 10 pairs of those little Scottie magnets that your kids play with and I threw a pair of magnets into the motherboards of all 10 computers and then closed the computers and asked the first computer to add 2 and 2 and it gives me ‘minus 5.’ Then I asked the second computer how much is 2 and 2 and it says, ‘Well over 3.’ The third one just whirs. The fourth one doesn’t do anything, and so on, for each computer, down the line.
“Now if we had computer epidemiologists they would look at these 10 computers and they’d say they are all sick and each appears to have a different disease, i.e., each gives a different wrong answer to the question how much is 2 plus 2. If the epidemiologists didn’t see me throw the Scottie magnets into the computer, they would say these are unrelated diseases. Not only that, but the incidence of the malfunction — each rendition of a wrong, but different answer to the question how much is 2 plus 2 — would not be significant enough to say there was any disease in the population at all because not enough of the computers gave the same wrong answer. That’s what we’ve got with brain-mediated, brain-damage disease and I would argue that one of the bases for Toxicant-induced Loss of Tolerance is brain-mediated damage.
“When you throw a neurotoxic chemical into the brain, and you know a lot of them get into the brain, including the limbic system, which is where the immune system, the nervous system, and endocrine system converge, they may make the brain misbehave in a number of different ways. One of the ways in which it may misbehave may be endocrine disruption. Another way that it may misbehave is attention deficit hyperactivity disorder (ADHD). A third way in which it may misbehave is that autism can develop.
“Now I said it was a thought experiment, but probably the organ we know the least about and which is computer central to our entire existence is our brain. Toxicant-induced Loss of Tolerance can manifest in a number of seemingly unrelated ways, unexplained by classical toxicology that assumes a one-hit or single insult resulting in a single kind of pathology.”
Tags:
ADHD,
attention deficit hyperactivity disorder,
computers,
emus,
environmental medical units,
limbic,
magnets,
National Academy of Sciences,
neurotoxic,
QEESI,
Quick Envionmental Exposure and Sensitivity Inventory,
tilt,
toxicant-induced loss of tolerance Category:
Health |
Comment
August 20, 2012, 6:31 pm
No time of year brings more changes for children and teens than the start of a new school year. They return to different classrooms and often entirely new schools. Classrooms may have been remodeled, repainted, recarpeted, or treated with pesticides.
These changes can affect children regardless of grade level — pre-kindergarten, grade school, high school and college. Amid the back-to-school excitement, some students wind up feeling sick, listless or distracted, unlike last year. And parents wonder why, and what they can do. Sometimes the school environment is the cause.
Understanding why your child feels bad is especially challenging with children who cannot tell you what may be going on at school. What to do? How about visiting the school yourself?
I have a personal example: My son was returning to fifth grade and for the first time was struggling in math and other subjects. When I visited his school on parents’ night, I was struck by the strong odor of new rubber-backed carpet that had been glued down throughout the school. The classrooms formerly had wood floors and windows that opened to let in fresh air. The goal of the remodeling was to reduce noise. But my son and many other children and teachers became ill when they returned to school after summer break. The most subtle and common symptom was difficulty concentrating and remembering, but headaches, fatigue and worsening asthma also occurred — all as a result of well-intentioned remodeling over the summer!
How can parents detect the early signs of TILT, or Toxicant-induced Loss of Tolerance? TILT is a process that starts with a chemical exposure, such as in a “sick building,” after remodeling at school or home, or from cleaning chemicals or a pesticide exposure. It can cause susceptible individuals to lose their tolerance for everyday substances that never bothered them before, frequently including foods! Intolerances people develop are not usual “allergies.” See a detailed explanation of the differences.
Here’s a 7-point guide for recognizing the early signs of TILT:
- Over long weekends or during vacations away from school does your son or daughter feel better? Do they feel better just being outdoors? Pay particular attention to symptoms that occur when your child returns to school after a vacation. Do headaches, migraines, irritability, or other symptoms such as tics or stomach problems diminish when they are away from the school? Do the symptoms return “with a vengeance” once they return to classes? This is a useful “experiment”: avoiding the school for a week or so while on vacation, and then returning, paying close attention to symptoms. Re-exposure can evoke a “sharp response,” making it clearer which symptoms are related to a particular environment. Sometimes the return to school after the summer provides the clearest evidence — keep a symptom log on a wall calendar.
- Did your child’s health problem(s) begin with a flu-like illness and fatigue that did not go away?
- Does your child, and do other children from the school, report symptoms involving multiple organ systems, with a predominance of neurological symptoms such as fatigue, memory and concentration difficulties, sudden overwhelming sleepiness, headaches, confusion, unsteadiness/clumsiness, irritability or depression? But also, digestive difficulties, skin rashes, muscle weakness, sinus and nasal symptoms, recurrent infections, breathing problems (e.g. asthma) etc., that have become more frequent since school began. School nurses often have a handle on this and can be helpful if approached in a non-confrontational way.
-
Since your child returned to school, has she had any adverse or unusual reactions to medications, such as antihistamine/decongestants, antibiotics, antidepressants, injections, or general or local anesthetics (for example, at the dentist’s office)? This is particularly significant if the drug was formerly well-tolerated. It is an example of “loss of tolerance” due to exposure.
-
Does your child report feeling ill after meals, or that she is unable to tolerate foods she formerly enjoyed? Does your child have intense food cravings or feel ill if she misses a meal. Must she eat “on time” and or does she feel ill if a meal is missed? Does your child raid the refrigerator at night, e.g., for ice cream or other foods, drink large quantities of milk or sodas (corn sugar), eat chocolate or other candy, cookies, bread, popcorn/corn chips, or other foods “addictively.” Does she feel terrible the next morning from her food addictants?
-
Does your child use caffeine? What happens if she doesn’t get her usual amount each day? Is she now using increased amounts of caffeine or, alternatively, avoiding caffeine because it bothers her? Overuse and avoidance can both be signs of caffeine intolerance. Avoidance leads to withdrawal symptoms. As with drugs, overuse may help postpone/overcome caffeine and food withdrawal.
- Is your child hypersensitive to: 1) noise (crowds yelling at sports events, vacuum cleaner); 2) bright light (closes blinds, uses sunglasses indoors); 3) vibration/touch as when someone bumps into their bed; or 4) certain odors.
Be sure to notice when symptoms occur and whether any particular exposures/odors may have preceded them. For example, do felt-tip markers, engine exhaust, fragrances, odorous cleaning products such as bleach, nail polish/remover, hair spray, and phenolic disinfectants (those whose names end in “-sol”) now make your child feel ill or trigger symptoms? Use EPA’s “Tools for Schools” to work with your school district to choose the least toxic cleaning and pest control approaches, e.g., integrated pest management where least toxic approaches are used first. Another excellent resource is the Healthy Schools Network website.
My tip to parents: Record symptoms on a calendar, along with where your child was that day, foods they ate, and symptoms such as dark eye circles (so-called “raccoon eyes”), headaches, nasal stuffiness or runny nose, fatigue, stomach ache etc., rating symptom severity on a 0-10 scale, with “5″ being moderate symptoms and “10″ severe or disabling. Seizures would be “10.”
For more information and a validated, diagnostic questionnaire on TILT, see the Quick Environmental Exposure and Sensitivity Inventory, or QEESI, that can be downloaded without charge from my website. Fill it out, score it, and take it to your doctor along with your calendar/graph of symptoms over time.
Tags:
"raccoon eyes",
"sick building",
allergies,
asthma,
back to school,
Chemical intolerance,
cleaning chemicals,
fatigue,
migraines,
neurological symptoms,
pesticide exposure,
phenolic disinfectants,
school,
school rooms,
tilt,
toxicant-induced loss of tolerance Category:
Health |
Comment